Everything you need to know about In vitro fertilisation (IVF)!
Published 6 Feb 2021 • By Candice Salomé
IVF enables many couples struggling with infertility to become parents. It is a type of assisted reproduction technology (ART).
But what does this method involve? Who can benefit from it? Are there any contraindications for people with chronic illnesses? What is its success rate?
We tell you everything in our article!

What is In vitro fertilisation?
IVF is a technique used by couples who wish to have a child and are facing infertility.
In Vitro Fertilisation consists of bringing the egg into contact with a sperm in the laboratory ("in vitro") in order to obtain good quality embryos that can lead to pregnancy after being transferred into the uterus.
The patient must first undergo controlled hormonal stimulation in order to obtain ovocytes which will then be fertilised in the laboratory where they will remain in culture for a few days.
One of the embryos will then be transferred to the uterine cavity. The others will be cryopreserved* for later use.
*Cryopreservation is a process in which whole cells or tissues are preserved by cooling them to a very low temperature, typically -196°C.
Who is eligible?
The first step for a couple who are having trouble conceiving is to consult a doctor who will assess the fertility of both the man and the woman. Whenever possible, the doctor will first treat either person's fertility so that they can restore their natural fertility.
If this is not possible, then certain methods will be used, such as ovulation stimulation with a prescription drug or artificial insemination. IVF is offered to couples for whom these methods have previously failed.
IVF is the treatment of choice for men or women who have been diagnosed with:
- Absent or blocked fallopian tubes
- Male infertility that could not be treated (low motility or low sperm count)
If ovulation induction or artificial insemination has failed, In Vitro fertilisation is recommended in the following cases:
- In women with endometriosis,
- In women with unexplained infertility,
- In women over a certain age, with poor egg quality.
IVF can also be performed for couples with genetic disorders that could lead to a serious health condition (such as myopathy, cystic fibrosis, neurofibromatosis, beta thalassaemia, retinitis pigmentosa, Becker's muscular dystrophy, haemophilia or Huntington's disease) so as to choose a healthy embryo.
Are there any contraindications for people with chronic illnesses?
Lupus: According to The Journal of Rheumatology, IVF is safe and effective for women with lupus in clinical remission. Although fertility is generally normal for lupus patients, when problems do arise these women can resort to IVF. Since IVF is based on hormone stimulation, this procedure may increase the risk of flare-ups.
Cancer: As chemotherapy, radiotherapy and surgery can damage the reproductive organs, cancer treatment can affect fertility. Women have a certain number of eggs, called the ovarian reserve. This reserve naturally decreases as time passes. However, some cancer treatments can diminish this reserve. Because of this, IVF is an option for cancer patients.
Multiple sclerosis: There is no decline in fertility in people with MS. However, in some people, regardless of their condition, fertility may be impaired. The PRIMS (Pregnancy in Multiple Sclerosis) study shows that using IVF can significantly increase the yearly rate of relapses within 2 months of the procedure:
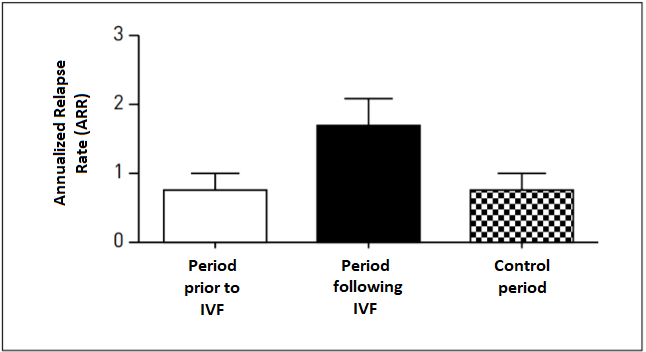 Annualized relapse rate based on 2-month periods before and after IVF
Annualized relapse rate based on 2-month periods before and after IVF
Source: Dr Claude Mékies (Toulouse), based on a paper by Professor Sandra Vukusic (Lyon)
This increase in flare-ups also has repercussions in the event of IVF failure:
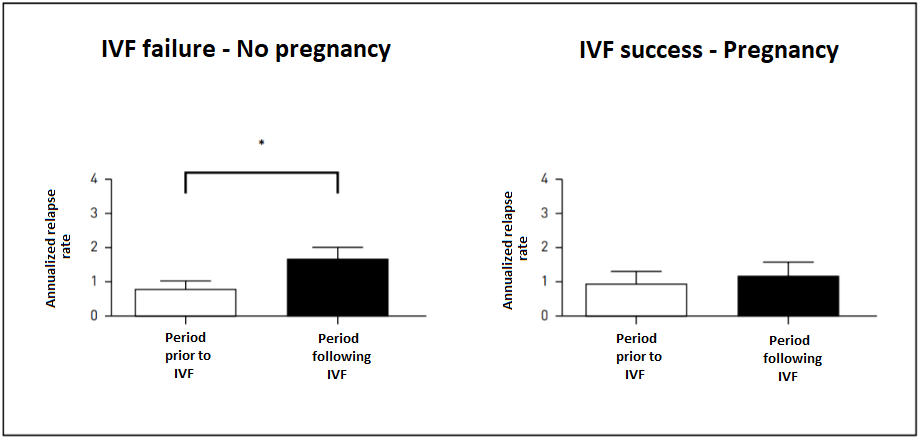
The annualized relapse rate increases significantly following IVF failure, whereas this is not the case in early pregnancy.
Source: Dr Claude Mékies (Toulouse), based on a paper by Professor Sandra Vukusic (Lyon)
What is the difference between conventional IVF and ICSI-IVF?
What we call "classic" in vitro fertilisation is the first technique ever used. In 1975, two pregnancies were achieved but did not result in a birth. In 1978, the first test-tube baby was born in England and then in 1982 in France.
Depending on the quality of the sperm collected, the doctor will recommend either classic IVF or ICSI (Intracytoplasmic sperm injection) IVF. Indeed, if the number of spermatozoa is insufficient, or if the sperm structure or motility is impaired, the use of ICSI IVF will be required.
The difference between conventional IVF and ICSI IVF is the method of fertilisation:
- Conventional IVF involves bring sperm and ovocytes into contact with each other in a nutrient liquid in a petri dish. This is placed in an incubator at 37°C until the next morning. The next day, all inseminated ovocytes are carefully and individually examined to see whether fertilisation has taken place. This technique is usually recommended in cases of female infertility. "Classic" IVF has the great advantage in that the gametes (reproductive cells) are left in the petri dish to fertilise on their own, so the selection remains natural.
- ICSI IVF was introduced to the UK in 1992.This technique uses the different stages of conventional IVF, but the fertilisation process is different. For ICSI IVF, a sperm cell is directly chosen and injected into the egg. In contrast to conventional IVF, after injection the ovocytes are prepared and placed in petri dishes. Once this step has been carried out, the same number of sperm and ovocytes are selected, bearing in mind that one sperm is required for one mature oocyte. Following the injection the steps for monitoring embryo development and implantation in the patient's uterus are the same as in conventional IVF.
What are the chances of success with in vitro fertilisation?
Every year in the UK, the Human Fertilisation and Embryo Authority (HFEA) tracks the success rates of IVF treatment. Fertility clinics and reproduction laboratories are required to transmit the results of their activities the HFEA.
When examining IVF success rates, it is important to understand exactly what is being measured. There are a number of angles from which to analyse the success of IVF: success per IVF cycle, per patient, per embryo transfer, or even per embryo transferred. It is also crucial to understand the definition of "success" - is it qualified as pregnancies or as live births?
HFEA has reported that the overall success rate (as defined as birth rate per embryo transferred) in 2018 was 23%, the highest it has ever been.
Rates tend to be higher when we talk about the success rate per transfer because we exclude from the calculation all the cycles in which the ovaries did not produce embryos that could be transferred. This generally results in a 30-35% success rate after transfer for patients below age 35.
Around 20,000 children born in the UK each year are a result of IVF, representing around 2% or births and certainly a triumph for parents and the medical field!
Was this article helpful to you?
Share your thoughts and questions with the community in the comments below!
Take care!
Sources:
- Qu’est-ce qu’une FIV ? FIV.fr
- La fécondation in vitro (FIV), Assistance médicale à la procréation
- La fécondation in vitro avec ICSI, Assistance médicale à la procréation
- L’assistance médicale à la procréation, Haut Conseil de Santé Publique
- Quel est le pourcentage de chances de réussite d’une FIV ?, Guide de l’infertilité
- Assistance médicale à la procréation (AMP), INSERM
- Fertility treatment 2018: trends and figures, Human Fertilisation & Embryology Authority

 Facebook
Facebook Twitter
Twitter


