What is oxygen therapy?
Published 8 Jan 2022 • By Clémence Arnaud
Oxygen therapy is a type of treatment aimed at providing oxygen by respiratory route. The number of patients undergoing oxygen therapy is constantly increasing in the UK.
What does oxygen therapy consist of? In what situations do patients need oxygen therapy? What are the different types of oxygen therapy? How to live normally when you need oxygen therapy?
We tell you everything in our article!

Different types of oxygen therapy
There are two types of oxygen therapy:
- Hyperbaric oxygen therapy: This is used only in special emergency situations such as decompression sickness or carbon monoxide poisoning, for example. Oxygen is administered at a higher than normal pressure in a specific chamber called a "hyperbaric chamber".
- Normobaric oxygen therapy: This type of oxygen therapy involves breathing oxygen through a medical device to improve the patient's ventilatory capacity. We will only discuss this type of oxygen therapy throughout the rest of this article.
Pulmonary gas exchange: How does it work?
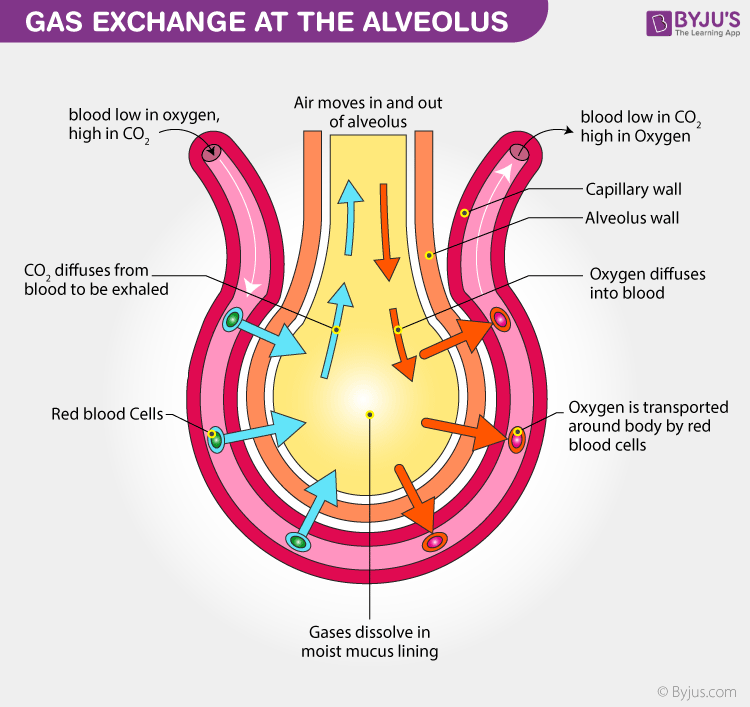 Source: Gas Exchange, Byjus
Source: Gas Exchange, Byjus
Gas exchange occurs from the place where the pressure is higher to the place where the pressure is lower. This is why oxygen (O2) will pass from the pulmonary alveolus to the blood and bind to haemoglobin. The O2 can then be distributed to the body's organs and allow them to function. When the blood returns to the lungs, it is highly charged with carbon dioxide (CO2), which will pass through the alveoli to be exhaled from the body.
When gas exchange is disturbed, two phenomena occur:
- Hypoxaemia: This refers to a lack of oxygen in the blood. It is defined when the oxygen pressure in the blood is <70 mmHg (millimeters of mercury).
- Hypercapnia: This is an excess of carbon dioxide in the blood. It is defined when the pressure of CO2 in the blood is >45 mmHg.
Both of these phenomena can have repercussions on all the organs of the human body. Poor blood oxygenation prevents the organs from functioning normally and may lead to multiple disorders. The direct consequences may include: difficulty breathing (dyspnoea), morning headaches, and chronic fatigue.
Oxygen therapy can be put in place to prevent hypoxaemia and hypercapnia in the long term.
When is oxygen therapy prescribed?
Arterial blood gases testing (ABG) can be used to determine if a patient has respiratory failure, the condition in which the lungs cannot take in sufficient oxygen or expel sufficient carbon dioxide to meet the needs of the cells of the body. Respiratory failure can be acute, chronic or intermittent (e.g. sleep apnea). Several health conditions may require oxygen therapy, the most common of which is chronic obstructive pulmonary disease (COPD).
COPD is a chronic inflammatory disease that affects the airways and more particularly the bronchi. The consequences of this condition are breathing difficulties with obstruction and narrowing of the airways. A destruction of the lung parenchyma called emphysema is often associated with COPD. COPD is only managed with oxygen in the most severe stages.
Other conditions are also treated with oxygen therapy, such as cystic fibrosis and interstitial lung disease. More recently, some patients with COVID-19 have been able to use oxygen therapy.
What are the different types of oxygen therapy devices?
Oxygen can be administered in different forms. After evaluating the patient's needs, a doctor may prescribe one of the following forms:
- A stationary device: These include concentrators, liquid oxygen, or compressed oxygen cylinders.
- A portable device (to facilitate use outside the home): Including, portable concentrators, portable liquid oxygen, or oxygen gas tanks.
The patient should also be equipped with a breathing system such as a nasal cannula (a device with two mouthpieces that allows oxygen to be delivered directly to the nostrils) or a face mask.
In the case of COPD care, oxygen concentrators are the most commonly used method of home oxygen therapy.
Oxygen therapy in practice
Oxygen therapy must be adapted according to the patient's lifestyle. There are 3 flow rates depending on the situation: flow rate at rest, flow rate during exercise and flow rate during sleep.
In addition, to obtain an optimal effect with this method, training remains a key element:
- Understanding treatment methods: flow rate, duration of daily use, using and maintaining the equipment,
- Re-evaluation of the prescription with a healthcare professional. In the case of stabilised diseases such as COPD, oxygen therapy should be prescribed for life.
Stopping smoking is a must when starting oxygen therapy. Smoking could negate the effects of oxygen and also lead to fires and burns.
There are many constraints associated with oxygen therapy, this is why the treatment should be thoroughly discussed with a healthcare professional.
Pulmonary rehabilitation
Pulmonary rehabilitation is a set of techniques and treatments to improve respiratory capacity. It is personalised according to the patient's needs and is carried out by several health professionals. This programme can be carried out in hospital, in a local facility (physiotherapy centre or doctor's surgery) or at the patient's home.
Pulmonary rehabilitation can be carried out when patients experience a decline in quality of life, for example, dyspnoea, a decrease in daily activities or intolerance to exercise despite appropriate treatment. It can be performed together with oxygen therapy
First of all, the patient's capacities at rest (spirometry) and during exercise (exercise ECG) should be assessed. It will also be necessary to make a clinical examination (to evaluate the degree of dyspnea, the quality of life, psychosocial factors...) as well as to evaluate the comorbidities. In order to provide the best possible care for the patient, it will be necessary to find the nearest respiratory rehabilitation centre and to ensure good coordination between all the health professionals involved.
The course consists of a minimum of 12 sessions. There are, on average, 20 sessions over a period of 6 to 12 weeks. In order to achieve a better recovery in the long term, it is important to continue the efforts for a period of 6 months to 1 year with regular and personalised exercise and a therapeutic education programme. In addition, and if necessary, dietary or psycho-social support, as well as respiratory physiotherapy can be recommended.
Breathing techniques for stress relief
Everyday life can sometimes be difficult to cope with, situations may occur that can interfere with therapy. Stress can often cause shortness of breath, or make it worse. It is important to learn to manage stress in everyday life, in order to avoid shortness of breath. Appropriate daily physical activity can help you manage your stress and breathe better. Breathing exercises can also be helpful.
Source: Positions to reduce shortness of breath - BPCO.org
While standing: bend forward slightly, with your hands on your thighs (the image on the left) OR bend forward with your elbows on the table and your neck relaxed (central image) OR slightly bend forward with your hands on the table (the image on the right).
Conclusion
Oxygen therapy is often viewed as a burdensome or demanding treatment for patients, but it doesn't have to be! With proper education and regular support from healthcare professionals, patients on oxygen therapy can live normal, fulfilling lives!
Would you like to read a Carenity member's experience with oxygen therapy? Read about Maria's journey with oxygen therapy, an O2 tank, and pulmonary rehab below:
Was this article helpful to you?
Give it a like and share your thoughts and questions with the community in the comments below!
Take care!
Sources:
Observatoire des données de l’Antadir - décembre 2015
Oxygénothérapie hyperbare et normobare, quelles différences - Orkyn
Les échanges gazeux - Alloprof
L’insuffisance respiratoire - La revue médicale suisse
Oxygénothérapie - Rapport d’évaluation de 2012 - HAS
Comment mettre en place une réhabilitation respiratoire pour les patients ayant une bronchopneumopathie chronique obstructive ? - HAS
Les positions du corps pour réduire l'essoufflement - BPCO.org

 Facebook
Facebook Twitter
Twitter

