What is the link between chronic inflammatory bowel disease (IBD) and eye disorders?
Published 8 Dec 2023 • By Claudia Lima
Inflammatory bowel disease (IBD) is characterised by inflammation of the lining of part of the digestive tract. Its symptoms have a major impact on the daily lives of those affected.
Some of these symptoms also have an impact on eye health. Indeed, more and more research has been finding links between IBD and various eye disorders.
So what are these links? What are the symptoms of eye disorders caused by IBD? How can they be managed?
Find all the answers in our article!
IBD and its most common symptoms
IBD, or chronic inflammatory bowel disease, is caused by a disturbance in the immune system. It accounts for 500,000 cases in the UK, and comprises Crohn's disease and ulcerative colitis (UC).
Crohn's disease affects the various segments of the digestive tract, from the mouth to the anus.Ulcerative colitis (UC) affects the rectum and colon.
Both diseases evolve through inflammatory flare-ups alternating with phases of remission, the main symptoms being:
- Abdominal pain,
- Diarrhoea (between 4 and 20 bowel movements per day),
- Faecal incontinence,
- Loss of appetite and weight loss,
- Extreme fatigue,
- Fever,
- Damage to the anal region (fissure, abscess).
However, a significant aspect of Crohn's disease and ulcerative colitis is their ability to trigger extra-digestive conditions. These are known as extra-intestinal manifestations.
According to statistics, in 20% of cases, patients develop such complications as arthritis, psoriasis, liver disease or eye problems (around 10%).
Eye disorders linked to IBD are increasingly being recognised.
Eye disorders triggered by IBD
Patients with Crohn's disease or ulcerative colitis (UC) may experience a wide range of symptoms in the gastrointestinal tract, but also in sensory organs such as the eyes.
The symptoms and disorders listed below offer valuable clues to the condition of the underlying IBD.
These eye disorders include:
Uveitis
This is an inflammation of the middle layer of the eye, the symptoms of which are redness of the eyes, sensitivity to light (photophobia), eye pain, tears, the sensation of floating bodies in the eye and blurred vision. Treatment includes steroids and, sometimes, immunosuppressive drugs.
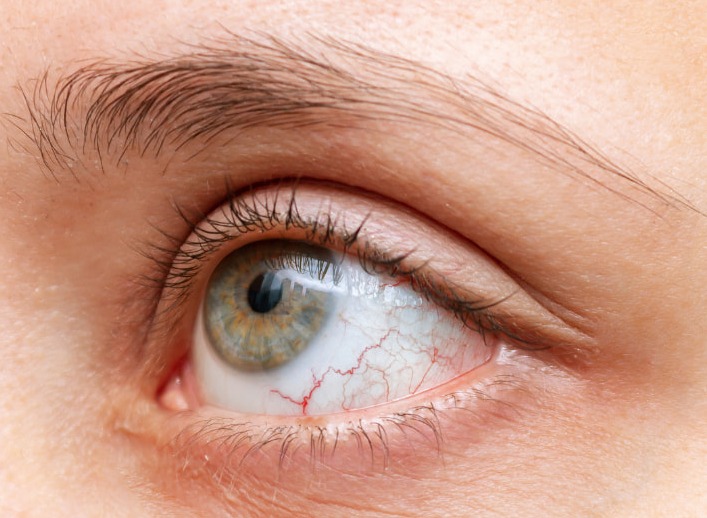
Episcleritis
It is an inflammation of the thin layer of tissue that covers the white of the eye, the episclera. Symptoms include red, swollen, watery and irritated eyes, a burning sensation and mild pain or discomfort. Episcleritis can disappear spontaneously or needs be treated with steroid eye drops.
Scleritis
If episcleritis does not disappear on its own or is poorly treated, scleritis develops. This is a severe and destructive inflammation of the sclera, the tough, fibrous white layer covering the eye, which can present a risk to the patient's vision. Symptoms include intense pain in the eye that worsens on palpation and radiates to the forehead, cheek or paranasal sinuses, as well as pronounced redness, increased eye sensitivity, heavy tearing and photophobia. A purplish-coloured erythema appears in part or all of the eye. Treatment begins with corticosteroids.
Other, more common eye disorders may also be associated with IBD, for example:
Conjunctivitis
This is an inflammation of the outer membrane of the eye, which may be caused by a microbial, chemical, allergic or inflammatory infection. To treat it, regular eye washing is recommended, along with eye drops and local care.
Bullous keratopathy
This condition involves a blister-like swelling of the cornea. Symptoms include sensitivity to bright light, blurred vision and a sensation of a foreign body in the eye.
Cataract
This is a progressive opacification of the crystalline lens. Symptoms include blurred or distorted vision, increased glare, sensitivity to light and double vision. Treatment consists of surgery to replace the opaque crystalline lens with a transparent artificial lens.
Dry eyes
Also known as dry eye syndrome, this condition is caused by poor quality or reduced production of tears. Symptoms include itchy or burning eyes, sensitivity to light, redness and blurred vision. Treatment consists of using artificial tears, applying warm compresses, massaging the eyelids and avoiding smoke and other irritants.
Why do patients with IBD develop eye disorders?
The exact cause of IBD-related eye conditions is still unknown.
More and more studies are pointing to a genetic component. A family history of Crohn's disease or ulcerative colitis (UC) is thought to increase the risk of ocular inflammation, even in people who do not suffer from IBD.
In addition, certain drugs used in the treatment of Crohn's disease or ulcerative colitis can cause eye problems. For example, oral steroids can cause various eye disorders, including glaucoma.
However, inflammation plays a central role in the link between IBD and eye disorders. The inflammatory processes that characterise IBD can spread beyond the gastrointestinal tract, affecting other parts of the body, such as the eyes. The immune cells activated during an IBD flare-up can migrate to ocular tissues, triggering a local inflammatory response.
Diagnosis and treatment of eye disorders in IBD
It is strongly recommended that you see an ophthalmologist at least once when you are diagnosed with Crohn's disease or ulcerative colitis (UC). And, of course, as soon as there is a slightest change in your vision. Early detection of IBD-related eye problems is crucial to effective management.
Treatment of IBD-related eye problems is often based on the overall management of the IBD itself. Anti-inflammatory treatments may be prescribed to reduce eye symptoms.
Here are some tips for minimising the symptoms of IBD-related eye problems:
- See an ophthalmologist, for a thorough eye examination,
- Stay hydrated, as dehydration can affect eye health,
- Eat a balanced, nutrient-rich diet, as certain nutrients such as vitamins A, C and E, as well as omega-3 fatty acids, are important for eye health,
- Rest your eyes, especially if you spend long periods in front of a computer screen or other electronic device,
- Protect your eyes from blue light, which can be very tiring. Use anti-blue light filters or anti-blue light glasses,
- Manage inflammatory flare-ups properly by following your treatment.
You should always see your healthcare professional for advice regarding your own situation.
Give it a "Like" and share your thoughts and questions with the community in the comments below!
Take care!

 Facebook
Facebook Twitter
Twitter


